Warning: This post discusses statistics about extreme pain that may be distressing. While cluster headaches are a neglected, high-impact issue, understanding their true burden requires appreciating the intensity of suffering involved. The pain often reaches levels far beyond typical human experience, making subjective accounts a valuable datapoint until we have robust methods for quantifying pain intensity. For further context, links to firsthand accounts are provided in the footnote.1
You no longer have a headache, or pain located at a particular site: you are literally plunged into the pain, like in a swimming pool. There is only one thing that remains of you: your agitated lucidity and the pain that invades everything, takes everything. There is nothing but pain. At that point, you would give everything, including your head, your own life, to make it stop.
- Yves, cluster headache patient from France (from Rossi et al., 2018)
Key Takeaways
- Cluster headaches are often considered among the most painful conditions known to medicine, if not the most painful (Nesbitt and Goadsby 2012). Patients describe the pain as “devilish”, “grueling”, “unbearable” or “so violent that it is utterly intolerable” (Torelli and Manzoni 2003), and rate it as significantly more painful than labor pain, gunshot wounds, or fractured bones, among others (Burish et al. 2021).
- Approximately 1 in 1,000 people worldwide will experience the excruciating pain of cluster headaches during their lifetime (Schindler and Burish 2022). In any given year, 1.5 million to 5.6 million (median: 3.0 million) adults are affected.
- We aggregated statistical data from a couple dozen papers on the prevalence, frequency, duration, and intensity of cluster headaches to estimate their global pain burden.
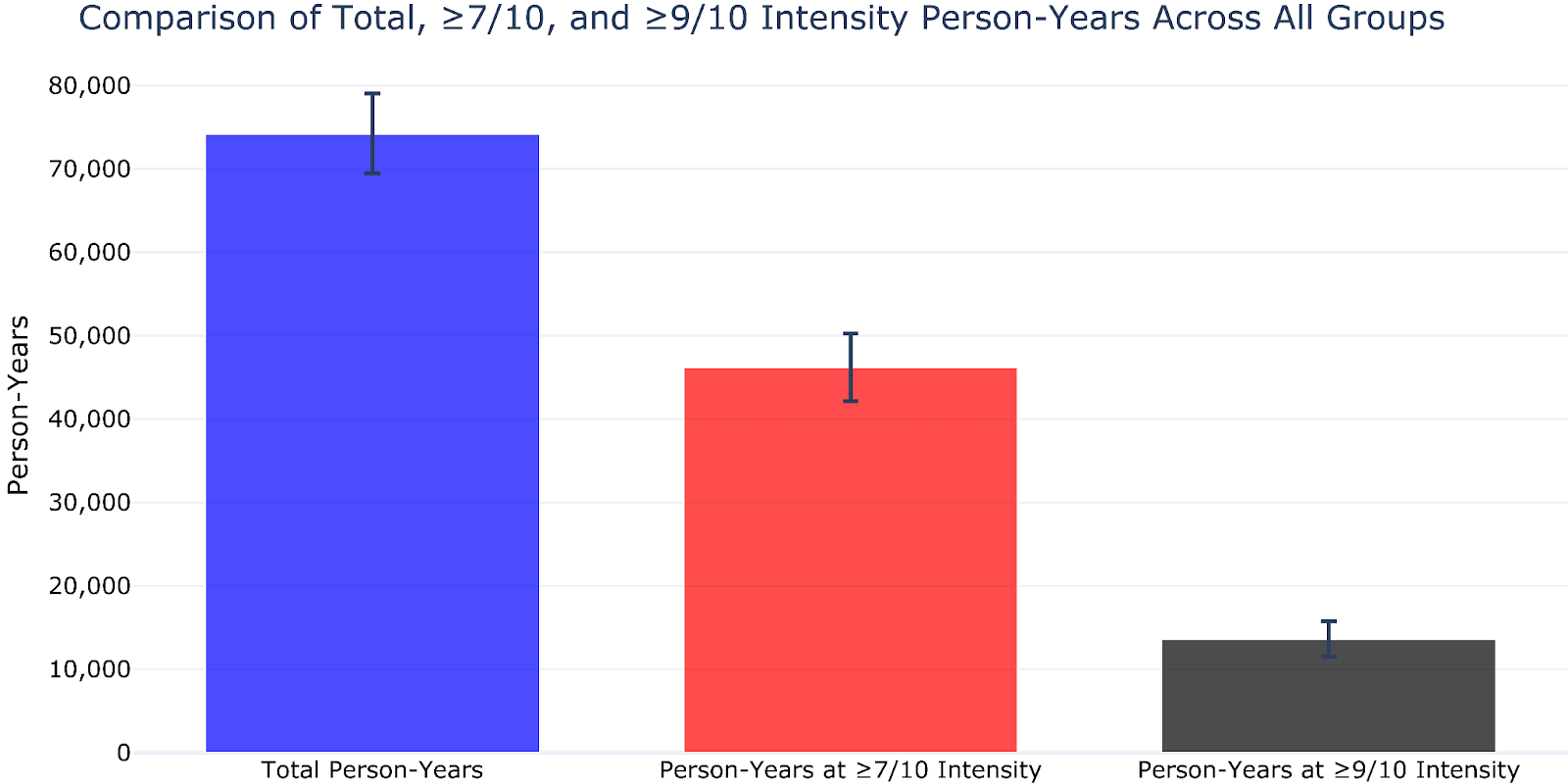
- We estimate that all cluster headache patients worldwide spend ~74,200 person-years per year in pain at any intensity, of which ~46,200 are spent at ≥7/10 pain and ~13,600 at ≥9/10 pain—that’s nearly 5 million person-days of extreme suffering (≥9/10 pain) annually.
- Drawing from research on the heavy-tailed nature of pain intensity (Gómez-Emilsson and Percy 2023), our numerical simulations show one way in which a straightforward aggregationist calculation2 means cluster headaches become a top global health priority. In particular, we compare the burden of cluster headaches with that of migraine, which is the 4th largest source of Years Lived with Disability (YLD) worldwide and 19th largest source of DALY (Disease Collaborative Network 2024).
- You can access the full simulations here: cluster-headaches.streamlit.app.
- The fact that the prevalence of cluster headaches is much lower than that of other major diseases is actually advantageous and presents an attractive opportunity: we can get rid of a significant proportion of the most extreme human suffering worldwide at a small fraction of the cost of addressing more prevalent conditions.
- Philanthropists, donors, charity and tech entrepreneurs, policymakers, and other decision-makers should consider cluster headache relief a strong contender for directing their altruistic efforts. This is particularly true for individuals who care about alleviating the most extreme forms of suffering, but the case can be compelling from nearly any ethical perspective.
1. Introduction
1.1. Clinical Features and Pain Comparisons
Cluster headaches (sometimes also referred to as “suicide headaches”) are a disorder characterized by attacks of severe pain behind the eye, typically lasting between 15 minutes and 3 hours (Black, Bordini, and Russell 2016). The onset of the attack is quite sudden, starting as mild discomfort and reaching maximal intensity on average within 9 minutes in 86% of sufferers (Torelli and Manzoni 2003). The pain is often described as similar to being repeatedly stabbed in the eye with a knife (Rossi et al. 2018; Schindler and Burish 2022). The term “cluster” refers to the fact that attacks come in bouts typically lasting 1–12 weeks, followed by periods of remission lasting a few months to a few years (episodic subtype) (Ekbom 1970). During a cluster bout, patients experience on average 3–4 attacks per day at predictable times of the day (Burish et al. 2021; Gaul et al. 2012), with a long tail extending to 10 attacks or more per day (Gómez-Emilsson 2019a; Sewell, Halpern, and Pope 2006). Up to 20% of cluster headache sufferers are of the chronic subtype, with remission periods shorter than 3 months (Schindler and Burish 2022).3 The ability of many patients to anticipate the timing of their attacks, both seasonally and daily, is perhaps one of the most sinister aspects of cluster headaches, adding a layer of psychological torment to the already excruciating pain.4
A recent international survey of 1,604 cluster headache patients revealed new data about how sufferers rate their pain compared to other severely painful conditions (Burish et al. 2021). Notably, respondents rated cluster headache pain as 9.7 ± 0.6 on a 0–10 scale, with 72% (n=1,157) rating it as 10.0. Respondents also rated other severely painful conditions they had experienced:
- Labor pain5 (n=308): 7.2
- Pancreatitis (n=30): 7.0
- Kidney stones (n=239): 6.9
- Gallstones (n=111): 6.3
- Gunshot wound (n=25): 6.0
- Disc herniation (n=261): 5.9
- Migraine attack (n=663): 5.4
- Fibromyalgia (n=63): 5.2
- Bone fracture (n=868): 5.2
It’s worth pointing out that these are all-things-considered, retrospective ratings, which means that individual attacks aren’t necessarily 9.7 painful on average. Indeed, studies show discrepancies in patients’ estimates of the duration and intensity of attacks between prospective reports (i.e., asking patients to report attack data in a diary right after the attack happens) and retrospective reports (i.e., relying on patients’ memory during interviews) (Snoer et al. 2018; Torelli and Manzoni 2003).
1.2. Treatment and Prevention
Treatment options for cluster headaches are limited and only partly effective. In the survey above, the most commonly used treatments were:
- Triptans (70%, n=1,119)
- Oxygen (67%, n=1,082)
- Opioids (34%, n=541)
Triptans were considered “completely effective” or “very effective” by 14% and 39% of those who use them, respectively; for oxygen, the numbers were 13% and 41%; and for opioids, only 1% and 4% (Pearson et al. 2019). Standard painkillers that can be effective against migraine and other types of headaches are ineffective against cluster headaches (Nesbitt and Goadsby 2012).
Indoleamines, and in particular tryptamines, have been found to be highly effective in both aborting attacks and helping patients go into remission, often indefinitely, after only a few low doses (Schindler and Burish 2022). A study of 53 patients who had used psilocybin or LSD found that:
- “twenty-two of 26 psilocybin users reported that psilocybin aborted attacks;
- 25 of 48 psilocybin users and 7 of 8 LSD users reported cluster period termination;
- 18 of 19 psilocybin users and 4 of 5 LSD users reported remission period extension” (Sewell, Halpern, and Pope 2006).
Another online survey of 270 cluster headache sufferers revealed that 68% of respondents who used tryptamines had a 4 or 5 out of 5 relief, with 5 being “completely eliminated the cluster headaches” (Frerichs 2019). The tryptamine N,N-DMT has been suggested as a potentially effective treatment due to its very fast action and requiring very low, sub-hallucinogenic doses. However, patients face major challenges accessing tryptamines due to their legal status, which has led to a proliferation of online communities discussing, e.g., ways to grow one’s own psilocybin mushrooms. Only very recently (June 2024), Canada approved the first psilocybin treatment for cluster headaches.
We recommend the 2020 policy paper “Legalising Access to Psilocybin to End the Agony of Cluster Headaches” by the Organisation for the Prevention of Intense Suffering (OPIS) for a more detailed overview of treatment options and policy recommendations, among others.
1.3. The Heavy-Tailed Valence Hypothesis and Existing Metrics
Descriptions of cluster headache pain are one of multiple lines of evidence in support of the “heavy-tailed valence” (HTV) hypothesis. This hypothesis posits that “the accessible human capacity for emotional experiences of pleasure and pain spans a minimum of two orders of magnitude” (Gómez-Emilsson and Percy 2023). The HTV hypothesis suggests that the difference between the mildest and most intense pain is not merely tenfold (as commonly interpreted when using the 0–10 scale) but rather spans a much broader range, with the most extreme experiences potentially being hundreds of times more intense than milder ones. In their survey (n=77), Gómez-Emilsson & Percy (Gómez-Emilsson and Percy 2023) found that 50% of respondents rated their most intense experience as at least twice as intense as the second most intense, lending support to the HTV hypothesis. Further lines of evidence in support of the HTV hypothesis are outlined in Gómez-Emilsson (Gómez-Emilsson 2019b).
Widely used health metrics such as the DALY (Disability-Adjusted Life-Year) are insensitive to these vast differences in our capacity to experience pain and pleasure. Recall that the DALY is calculated as the sum of years of life lost due to premature death (YLLs) and years of healthy life lost due to disability (YLDs), i.e., DALY = YLL + YLD. Since headache disorders are not considered a cause of death according to the Global Burden of Disease (GBD), YLL is zero and DALY = YLD (Stovner et al. 2018). Headache YLDs are then calculated as the product of the number of people with headaches worldwide, the average time spent with headaches, and, crucially, a 0–1 weight measuring the degree of disability caused by headaches, where 0 = full health and 1 = death. For instance, the disability weight for migraines according to the GBD is 0.44, whereas cluster headaches are not included at all due to their relatively low prevalence (“Global Burden of Disease Study 2021 (GBD 2021)” 2021)6. As (Stovner et al. 2018) points out:
“Although other headache disorders such as cluster headache undoubtedly impose a great burden on individual patients, the total societal burden of this and other severe but relatively rare headaches is probably quite small compared with that of the common headache types.”
As (Leighton 2023) has pointed out, there’s a need for alternative metrics that adequately capture the nature of suffering, especially at the extremes. Leighton argues that the Wellbeing-Adjusted Life-Year (WELLBY) (Frijters et al. 2024) and the Suffering Intensity-Adjusted Life-Year (SALY) (Knaul et al. 2018) are steps in the right direction but do not suffice, suggesting instead two potential metrics:
- Years Lived with Severe Suffering (YLSS): capturing suffering at the level of approximately 7/10 and above.
- Days Lived with Extreme Suffering (DLES): for suffering of approximately 9/10 and above.
There are several possible explanations why cluster headaches currently receive relatively little attention within the effective altruism community and more broadly. Some include:
- As noted above, the prevalence of cluster headaches is much lower than that of other sources of DALY, and current health metrics are largely insensitive to extreme suffering.7
- Cluster headaches rarely cause death (except in cases of suicide).
- Cluster headache attacks are not as visually gruesome as other conditions that may evoke stronger feelings of empathy (i.e., there’s typically no blood, severe wounds, or visible deformities involved).
- The fraction of the EA community that prioritizes extreme suffering remains comparatively small, and a sizable fraction of people and organizations who do prioritize suffering (understandably) focus on s-risk or animal welfare instead.
- The name “headache” underplays the extreme severity of the pain.
- The HTV hypothesis is not widely known or taken sufficiently seriously, resulting in an underestimation of the severity of extreme pain.
- There is limited research on the cost-effectiveness of different interventions to treat cluster headaches and of the (very few) organizations working behind them.
- Some of the most promising interventions, such as indoleamines, remain illegal in many jurisdictions, so carrying out such work requires the support of less risk-averse philanthropists.
1.4. Goal
The goal of this study is to estimate the annual global burden of cluster headache pain according to different metrics. We aggregate statistical data from the medical literature into a numerical model available at cluster-headaches.streamlit.app (full code). We then compare our results with the burden of migraine, the 4th largest source of Years Lived with Disability worldwide (Disease Collaborative Network 2024). We show under which assumptions and metrics cluster headaches result in a larger burden than that of migraines, which lends itself to useful comparisons and is significantly more prevalent. In particular, we find that a straightforward aggregationist approach that weighs the most severe pain (10/10) four orders of magnitude more heavily than the mildest pain (1/10) results in a higher total annual burden for cluster headaches. However, we also estimate that cluster headaches cause about 5 million Days Lived with Extreme Suffering (at ≥9/10 pain) per year, so individuals who prioritize reducing extreme suffering may be convinced to tackle this problem regardless of whether they believe it “outweighs” less severe but more prevalent pain.
We conclude with some suggestions for philanthropists, donors, policymakers, and other relevant decision-makers who take the HTV hypothesis seriously or otherwise put more weight on alleviating the burden of extreme suffering.
2. Methods
We’d like to answer the question: How much time is spent globally per year with cluster headache pain, at different pain intensities? So we need to estimate the following quantities:
- Prevalence: How many people worldwide suffer from cluster headaches in a given year?
- Frequency: How many attacks per year do cluster headache sufferers experience?
- Duration: How long do attacks last?
- Intensity: How painful are the attacks?
Each of these quantities will follow a certain probability distribution. We can then calculate the resulting burden distribution as:
Burden = Prevalence × Frequency × Duration × Intensity
We can then derive relevant metrics, such as YLSS and DLES. Finally, we can compare these metrics for cluster headaches with other conditions. For this report, we chose migraine, which lends itself to useful comparisons and is significantly more prevalent.
We find it helpful to distinguish between four different types of cluster headache patients, depending on whether they are chronic vs episodic, and whether they have access to treatment (either preventative or abortive) or not. This distinction can help us see how the burden is distributed among the groups and potentially prioritize them accordingly.
2.1. Prevalence
Level of confidence in the data: Medium
The literature presents a somewhat complex picture of cluster headache prevalence, with reported prevalence rates varying somewhat. Individual studies have reported 1-year prevalence rates as low as 0 (in Malaysia) and 32 (in Ethiopia) per 100,000, and as high as 150 per 100,000 (in Germany). A meta-analysis by (Fischera et al. 2008) of all available epidemiological studies (16 papers) estimated the 1-year worldwide prevalence at 53 per 100,000 (CI 26, 95), with the lifetime prevalence being 124 per 100,000 (CI 101, 151) for adults8 of all ages and sexes. They note that cluster headaches might be less frequent in developing countries, which more recent studies from previously understudied regions seem to confirm (Kim et al. 2023). This could bring the figure of 53 per 100,000 down slightly. Underdiagnosis and misdiagnosis complicate the picture further (Bahra and Goadsby 2004).
For our simulations, we use the default figure of 53 per 100,000, but the user can change this parameter.
The default value used for the fraction of chronic patients is 20% (vs 80% episodic), taken from the meta-analysis by (Schindler and Burish 2022).
2.2. Frequency
Level of confidence in the data: High
Multiple studies have documented the frequency of cluster headache attacks in detail. For episodic patients who typically experience annual bouts lasting a few weeks, ample data exist on the frequency and duration of the bouts. For our simulations, we considered the following:
- Bout frequency (episodic patients): We aggregated data from 7 papers (Ekbom 1970; Friedman and Mikropoulos 1958; Gaul et al. 2012; Kudrow 1980; Li et al. 2022; Manzoni et al. 1983; Sutherland and Eadie 1970), weighted them proportionally to the sample size in each paper, and fitted them to a discrete distribution.
- Bout duration (episodic patients): We aggregated data from 8 papers (Ekbom 1970; Friedman and Mikropoulos 1958; Gaul et al. 2012; Lance and Anthony 1971; Li et al. 2022; Manzoni et al. 1983; Rozen et al. 2001; Sutherland and Eadie 1970), weighted them proportionally to the sample size in each paper, and fitted them to a lognormal distribution.9
- Active days (chronic patients): Since chronic patients have attacks all year long with short or no remission periods, we modeled the days of attacks in a given year as a lognormal distribution with parameters such that (a) we avoid having patients with an improbably low number of attacks per year (e.g., fewer than 10) while (b) allowing for the possibility of a small fraction of patients having attacks almost every day.10
- Attacks per day: (Gaul et al. 2012) conveniently distinguish between chronic and episodic patients in their large study of 209 German patients, most of whom we assume have access to treatment since they were recruited in a specialized headache clinic. The mean (SD) values reported are 3.1 (2.1) for episodic patients (during bouts) and 3.3 (3.0) for chronic patients. Access to treatment can reduce the frequency of attacks, but we could not find clear data on the effect size. For our simulations, we assume 3.26 (2.21) for untreated episodic patients and 3.46 (3.15) for untreated chronic patients. Given (a) observations that patients can have days with more than 10 attacks (Sewell, Halpern, and Pope 2006) and even up to 20 attacks (Lademann et al. 2016), and (b) that the median number of daily attacks tends to be lower than the mean (see e.g., (Cho et al. 2019)), we modeled daily attack frequency as a lognormal distribution11.
2.3. Duration
Level of confidence in the data: High
The duration of each attack has also been well documented (Bahra, May, and Goadsby 2002; Russell 1981; Snoer et al. 2018). Most attacks last between 15 minutes and 3 hours, with 4–13% of patients reporting attacks longer than 3 hours (Kim et al. 2023). Attacks tend to be somewhat shorter at the beginning and end of a cluster period (Black, Bordini, and Russell 2016). Additionally, the onset and offset of each attack are quite sudden, reaching peak intensity within just 8.9 minutes on average and subsiding similarly quickly (Torelli and Manzoni 2003).
Less well documented is how the duration of an attack depends on factors such as the patient being episodic or chronic, whether patients have access to treatment (either preventative or abortive), or the intensity of the attack. In our model, we start with typical durations and incorporate the following adjustments:
- Attacks seem to be slightly longer for chronic patients (Cho et al. 2019; Snoer et al. 2018).12
- Access to treatment can reduce the attack duration (Gaul et al. 2012).13
- More painful attacks tend to be longer (Hagedorn et al. 2019; Russell 1981).
2.4. Intensity
Level of confidence in the data: Medium-low
We’re interested in modeling the distribution of time spent at different pain intensities on the 0–10 scale. The main challenge in answering this question is that most studies rely on retrospective reports (i.e., by interviewing or surveying patients about their attacks generally) as opposed to prospective reports (i.e., by asking patients to record the intensity in a diary immediately after the attack). We found three studies14 asking patients to record the intensity of their attacks in a diary. The results are summarized in Table 1 below.
| Study | Cohort details | Results |
|---|---|---|
| Russell (1981) | 24 patients recorded n=77 attacks 23 episodic, 1 chronic 22 men, 2 women No attacks were treated Attacks rated on a 1–5 scale |
- Extremely severe (5/5): 23 (30%) - Severe (4/5): 17 (22%) - Moderate (3/5): 20 (26%) - Slight (2/5): 5 (7%) - Very slight (1/5): 12 (15%) Mean: 3.44, SD: 1.39 |
| Torelli & Manzoni (2003) | 42 patients recorded one “typical” attack 42 episodic, 0 chronic No attacks were treated Attacks rated on a 0–10 scale |
- 9.0–10: 29 (69%) - 8.0–8.9: 7 (17%) - 7.0–7.9: 3 (7%) - 6.0–6.9: 3 (7%) Mean: 9.17, SD: 1.0 |
| Snoer et al. (2019) | 57 patients recorded a total of 500 attacks 24 episodic, 33 chronic 32 men, 25 women 54 (95%) patients used abortive treatments; 423 (85%) attacks were treated with abortives Attacks rated on a 0–10 scale |
- Median (IQR), treated attacks (n=423): 7.3 (5.9–8.7) - Median (IQR), untreated attacks (n=77): 7.0 (5.0–8.4) |
Table 1: Data from prospective studies of cluster headache pain intensity.
To model the pain distribution for untreated attacks, we fitted a truncated (at 10/10) normal distribution with the combined data from (Russell 1981) and (Torelli and Manzoni 2003). The truncation introduces some artifacts into our calculations, discussed in greater detail in Section 3.3, but we’ll limit the scale to 10 to align with established medical practice. For treated attacks, we fitted a truncated normal distribution to the (Snoer et al. 2018) data. Since the three papers likely underestimate the frequency of mild attacks, we adapted the distributions to increase the density of mild attacks.
Finally, to model the time profile of each single attack, we assume that the onset and offset each last 15% of the total attack time, and the remaining 70% is spent at the maximum pain intensity (sampled from the distributions above). While this simplification ignores fluctuations in pain, we believe it is a good approximation given observations by (Nesbitt and Goadsby 2012)15 and (Ekbom 1975).16
2.5. Burden Metrics
Our simulations calculate the average time spent at different pain intensities on the 0–10 scale, in steps of 0.1, for a representative sample of each of the four patient groups. We then extrapolate these results by multiplying the average time with the total global prevalence to arrive at the global burden (as a function of pain intensity). We can then derive a few metrics from this distribution. We focus on three, all global and annual:
- Person-Years in Pain17: the sum of person-years spent at all pain intensities, optionally weighing more intense pain more heavily, either linearly or nonlinearly (more below);
- (Person-)Years Lived with Severe Suffering (YLSS): as introduced by (Leighton 2023), the sum of person-years spent at ≥7/10 intensity, again with the option of weighing more intense pain more heavily;
- (Person-)Days Lived with Extreme Suffering: captures pain at ≥9/10 intensity.
We want to point out an important distinction between pain and suffering, which are correlated but different. Indeed, it is possible to experience intense pain with high equanimity, which reduces the suffering caused by the experience. The expression Suffering = Pain × Resistance, where resistance is the inverse of equanimity, can serve as a good first approximation (young2016pain?). However, we believe that pain and suffering correlate strongly at the very top of the scale. That is, no amount of equanimity can fully get rid of the suffering caused by pain near or at 10/10. So at least for ≥9/10 pain, we will use “pain” and “suffering” interchangeably, while noting that there is room for more research on this question.
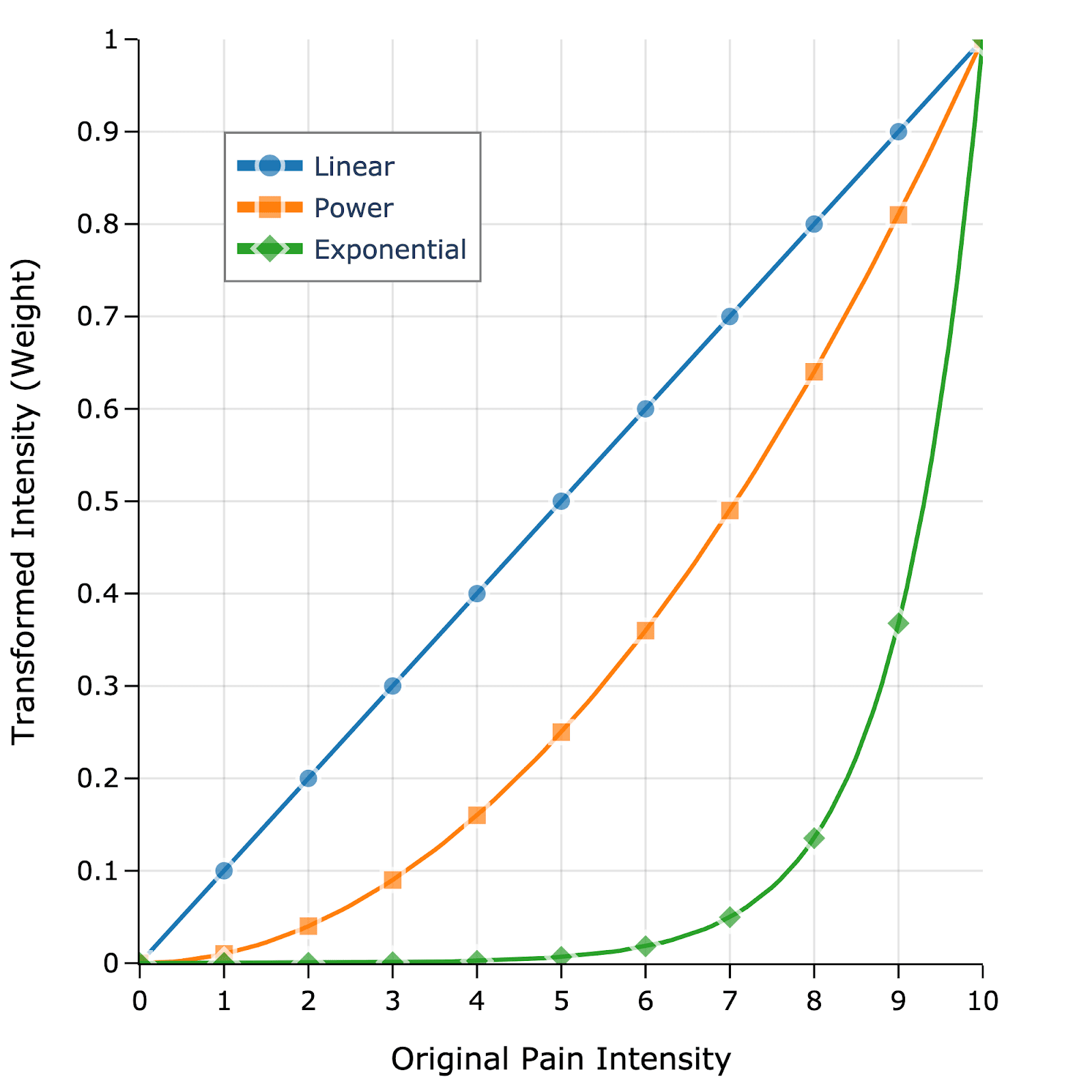
Our simulations let the user define how to weigh more intense pain relative to mild pain. Figure 1 shows three different options:
Mapping the pain scale linearly to a 0–1 weight has been proposed by (Stovner et al. 2018) as a way to approximate the disability weight of different types of headaches for DALY calculations. However, this ignores data suggesting that very intense pain is experienced as significantly more intense than what a linear scale might suggest (Gómez-Emilsson 2019b; Gómez-Emilsson and Percy 2023). Power and exponential weights might reflect this fact better while noting that there could be other possible transformations.
3. Results
The full simulation results can be accessed at cluster-headaches.streamlit.app.
3.1. Global Burden of Cluster Headache Pain
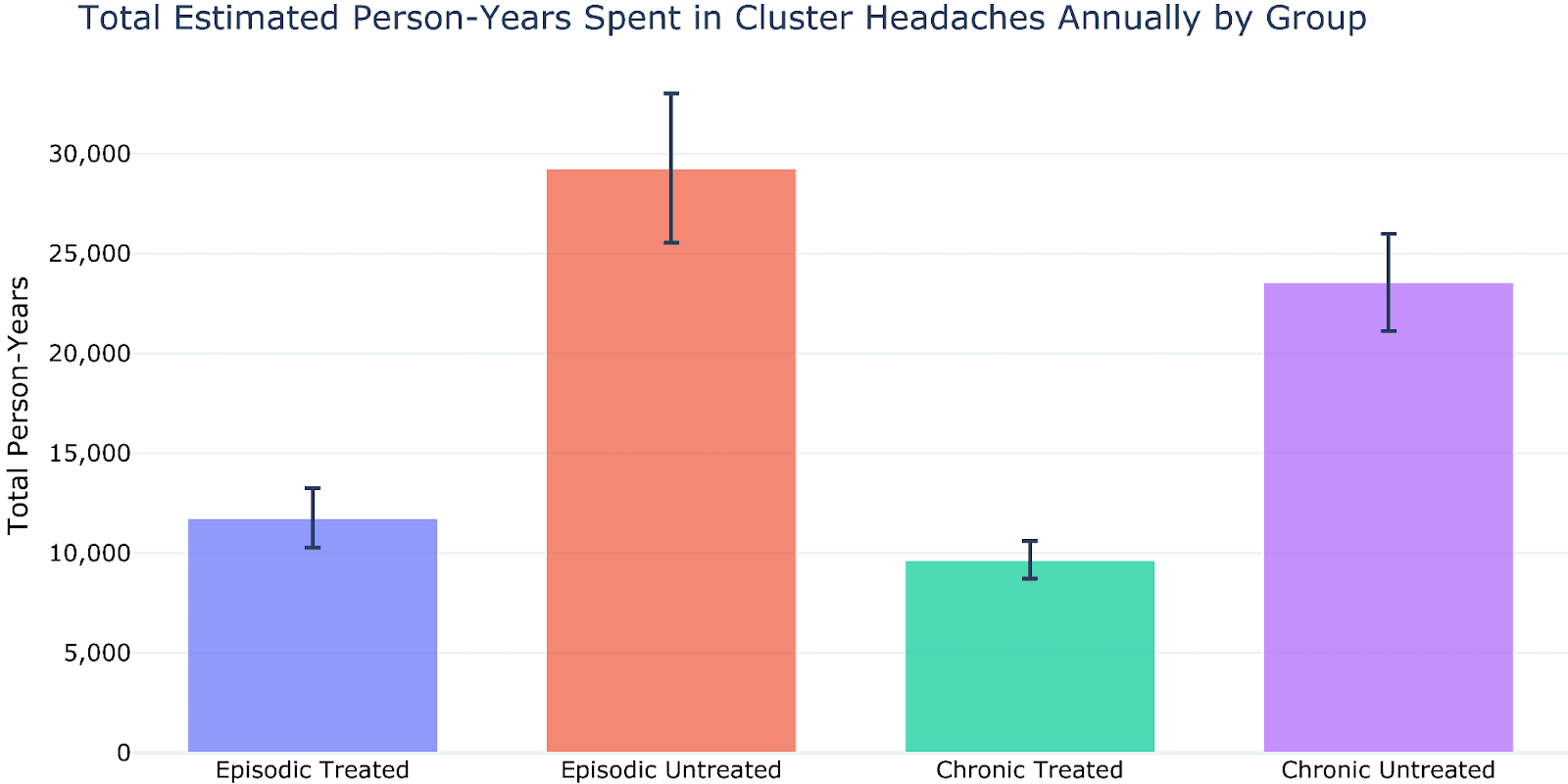
We ran Monte Carlo simulations for four different groups of cluster headache patients, depending on whether they are of the chronic vs episodic subtype, and whether they have access to treatment (preventative or abortive) or not. We assume that 20% of patients are chronic and 80% are episodic, and that 43% of patients worldwide have access to treatment.18 We simulated a total of 3,036 individuals and extrapolated the results of this sample population to estimate the total global burden.
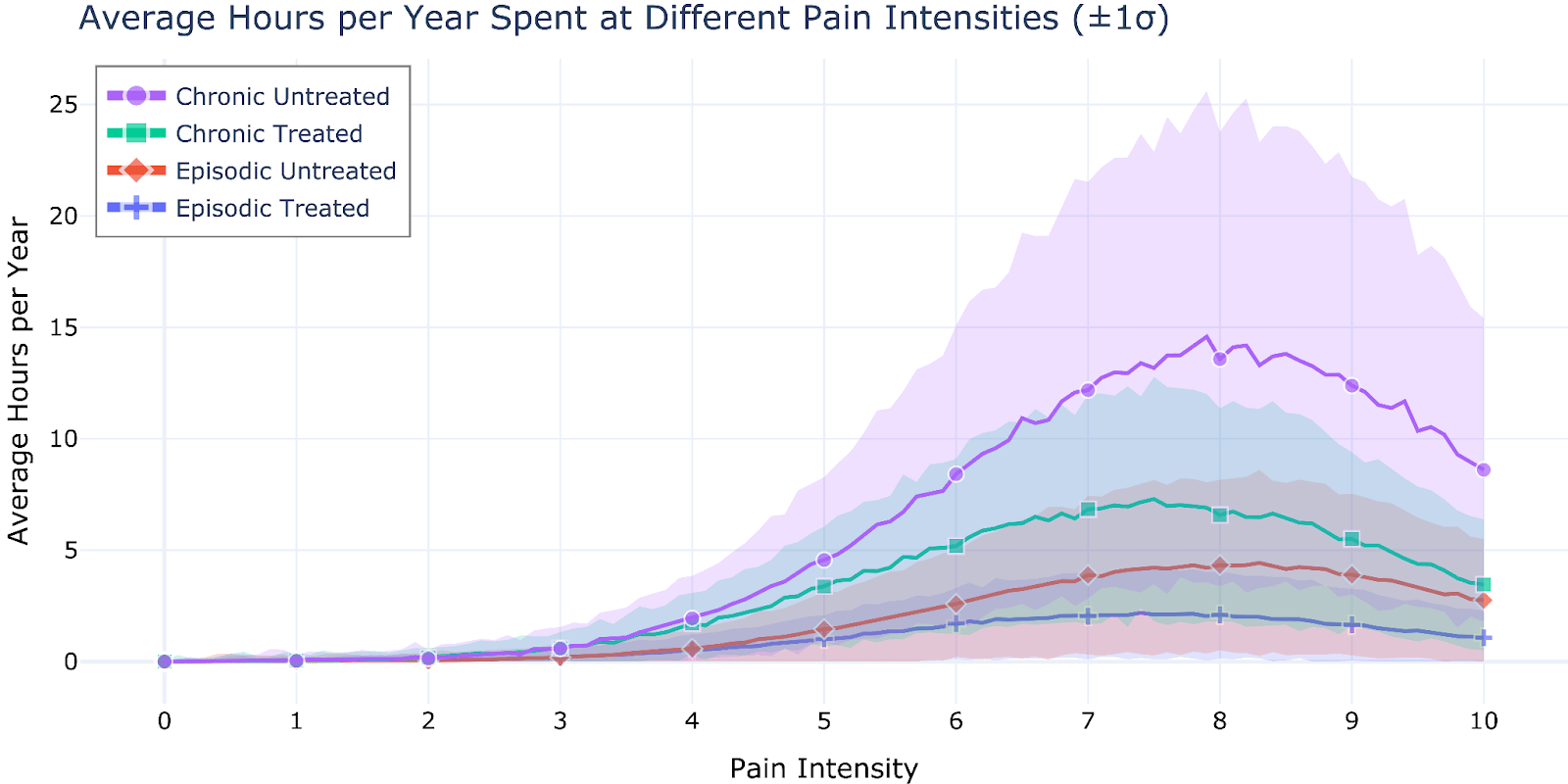
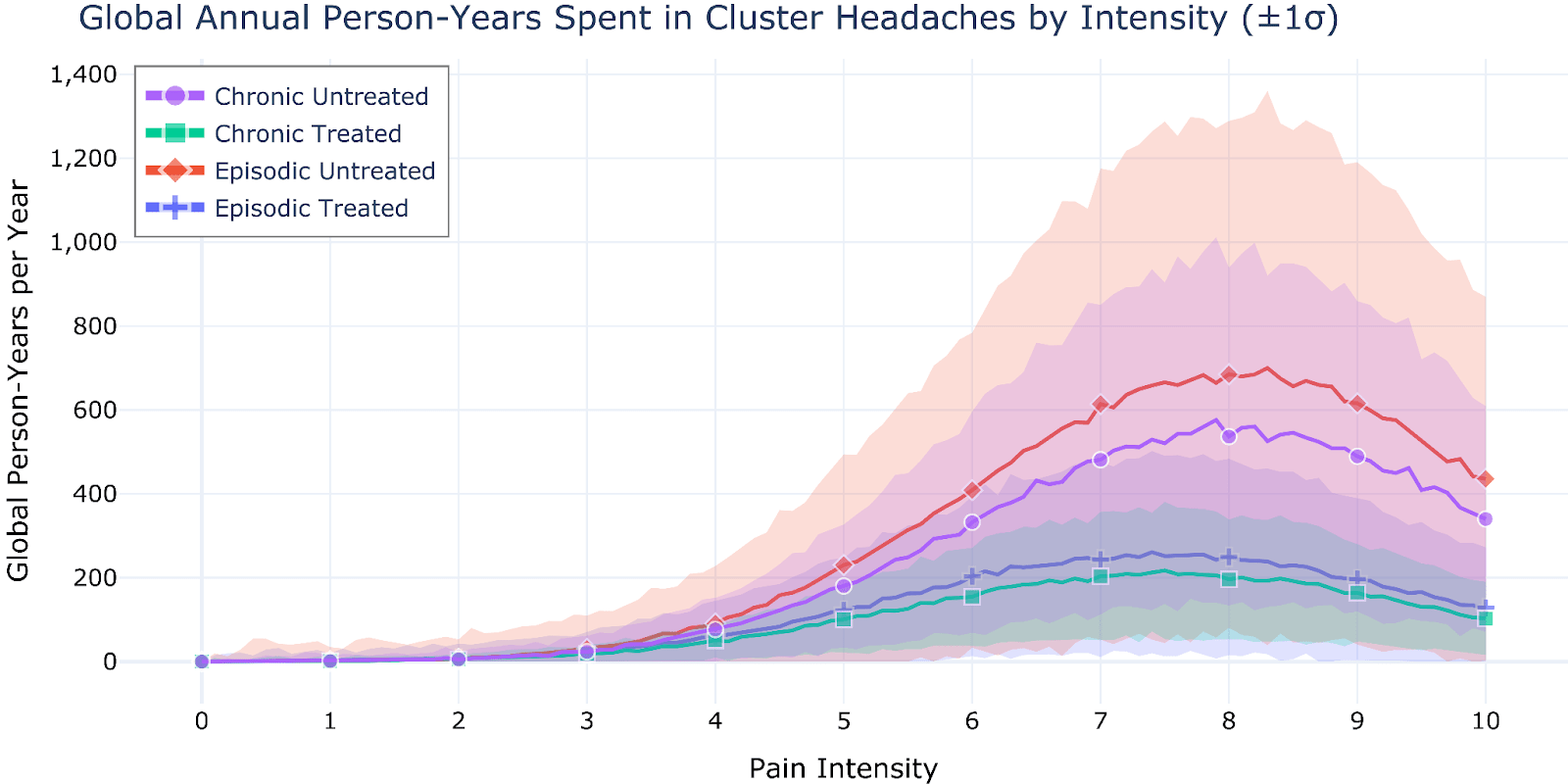
Figure 2 summarizes our main results. On average—and as expected—patients of the chronic subtype without access to treatment will spend the most time in cluster headache pain annually—596 hours per year, compared to 99 hours for the average episodic patient with access to treatment (Figure 2a). However, since the episodic subtype is ~4x more common than the chronic subtype, the total global burden is dominated by the episodic untreated group (Figures 2b,c). We estimate that all cluster headache patients worldwide spend ~74,200 person-years per year in pain at any pain intensity, of which ~46,200 are spent at ≥7/10 intensity and ~13,600 at ≥9/10 intensity (Figure 2d). Using the terminology introduced by (Leighton 2023), the figure of 46,200 person-years would correspond to the Years Lived with Severe Suffering (YLSS) for cluster headaches. The Days Lived with Extreme Suffering (DLES) would then be 13,600 years × 365 days/year = 4,964,000.
3.2. Reweighting of Extreme Pain
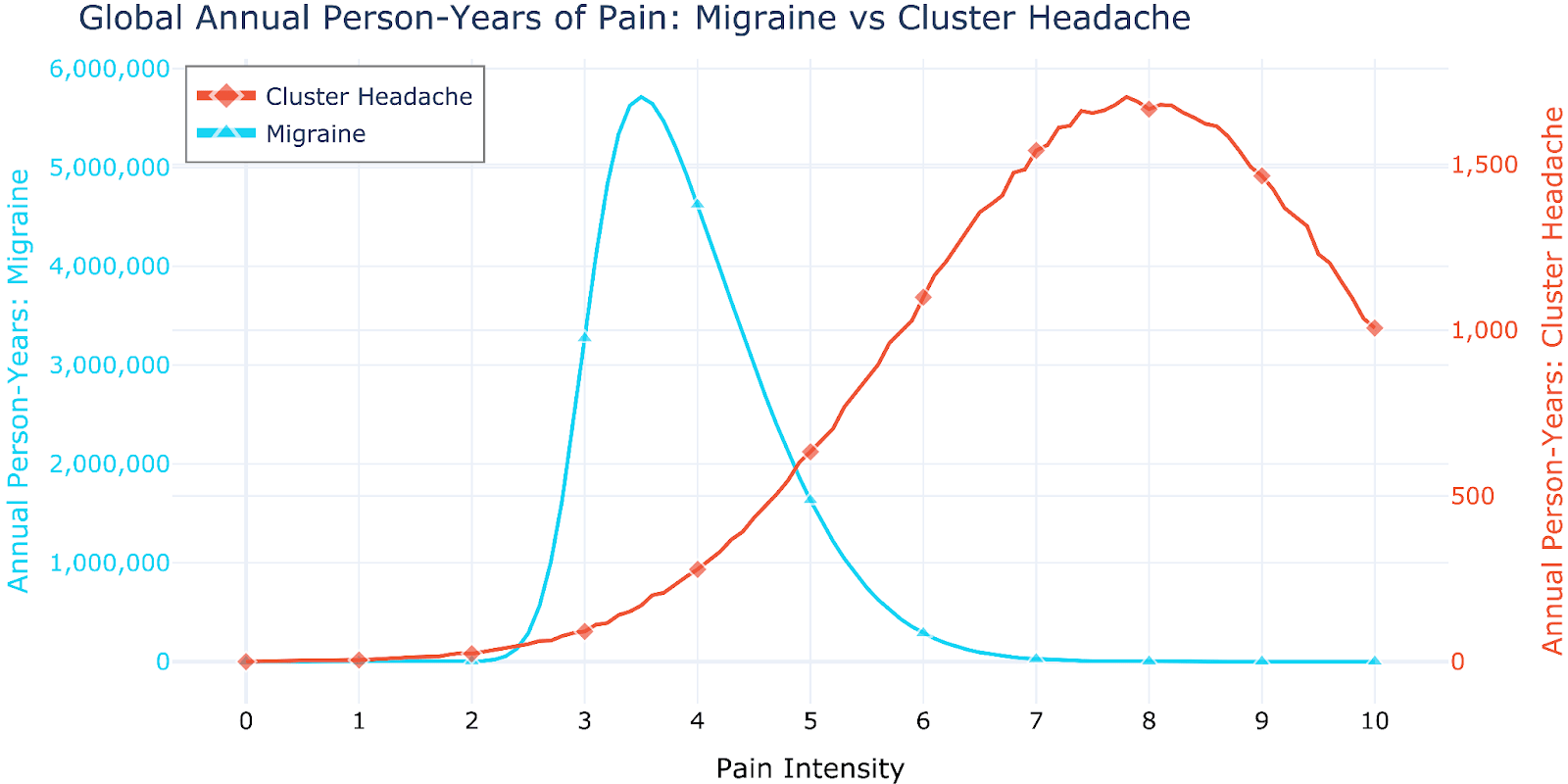
We now explore ways to give larger weight to more extreme pain, a consequence of accepting the heavy-tailed valence hypothesis. For illustrative purposes, we compare the global burden of cluster headaches to that of migraines.
- Approximately 14% of the world population suffers from migraines annually—a total of 1.158 billion people according to the latest estimates of the Global Burden of Disease report for 2021 (Disease Collaborative Network 2024).
- In 2021, migraines were the 19th largest source of DALYs (43 million19) and the 4th largest source of YLDs worldwide (behind low back pain, major depression, and age-related hearing loss).
- ~3 million people worldwide suffer from cluster headaches annually (2–3 orders of magnitude fewer than migraines). Additionally, (Stovner et al. 2018) estimates that the number of hours migraine sufferers spend in attacks as a fraction of the year is 8.5%—about 3.5 times more than cluster headache patients, who we estimate spend on average 2.4% of their annual time in pain. These differences in prevalence mean that cluster headaches do not even appear as a separate category in the Global Burden of Disease Report.
To compare our cluster headache burden results (Figure 2) with the burden of migraines, it would be necessary to know the distribution of time spent in migraine pain at different intensities on the 0–10 scale. One crucial challenge in doing so is that migraine sufferers who have not experienced more extreme forms of pain might overestimate the pain intensity of migraines. While severe migraines can indeed be very painful, it is generally acknowledged that severe cluster headaches are much more painful. As (Torelli and Manzoni 2003) point out:
“Literature reports and clinical practice suggest that the adjective ‘severe’ is inappropriate to describe the intensity of pain in CH, which cannot be compared to that of migraine either in quality or quantity.”
Additional evidence in support of this argument stems from the fact that cluster headache patients “appear agitated, restless, and feel an impulse to move around or go outside in an attempt to cope with the torment of excruciating pain” (Black, Bordini, and Russell 2016). During very severe attacks, “subjects may strike their heads on the wall or with their hands” (Black, Bordini, and Russell 2016). Contrast this behavior with that of migraine patients, who typically avoid movement, lie down or rest, or might want to ‘sleep it off’—forms of passive coping that the severity of cluster headache pain renders impossible.
In exploring this question, we consulted Dr. Mark J. Burish, Neurologist and Pain Medicine Specialist at UTHealth Houston and 1st author of the largest international survey of cluster headache patients (Burish et al. 2021). In his questionnaire:
- 1,604 patients rated cluster headache pain as 9.7/10 (mean; the median was 10, with IQR 9.6–10).
- 72.1% (1,157/1,604) rated cluster headache pain as 10/10.
- Only 1.1% (12/1,604) rated it as below 8.0.
- 663 patients also suffered migraines, and the mean pain score they assigned to migraines was 5.4.
- 506 of the 663 patients rated cluster headache pain as 10/10, none of the 506 rated migraine pain at 10/10, and only 8/506 rated migraine pain as ≥9/10.20
Given our uncertainties as to how to best model the underlying intensity distribution of migraines, in our simulations, the user can specify the shape parameters of a skewed normal distribution. As an illustrative example, assuming a distribution with a median of 4.2, mean of 3.0, and SD of 1.2, we arrive at the distribution shown in Figure 3.
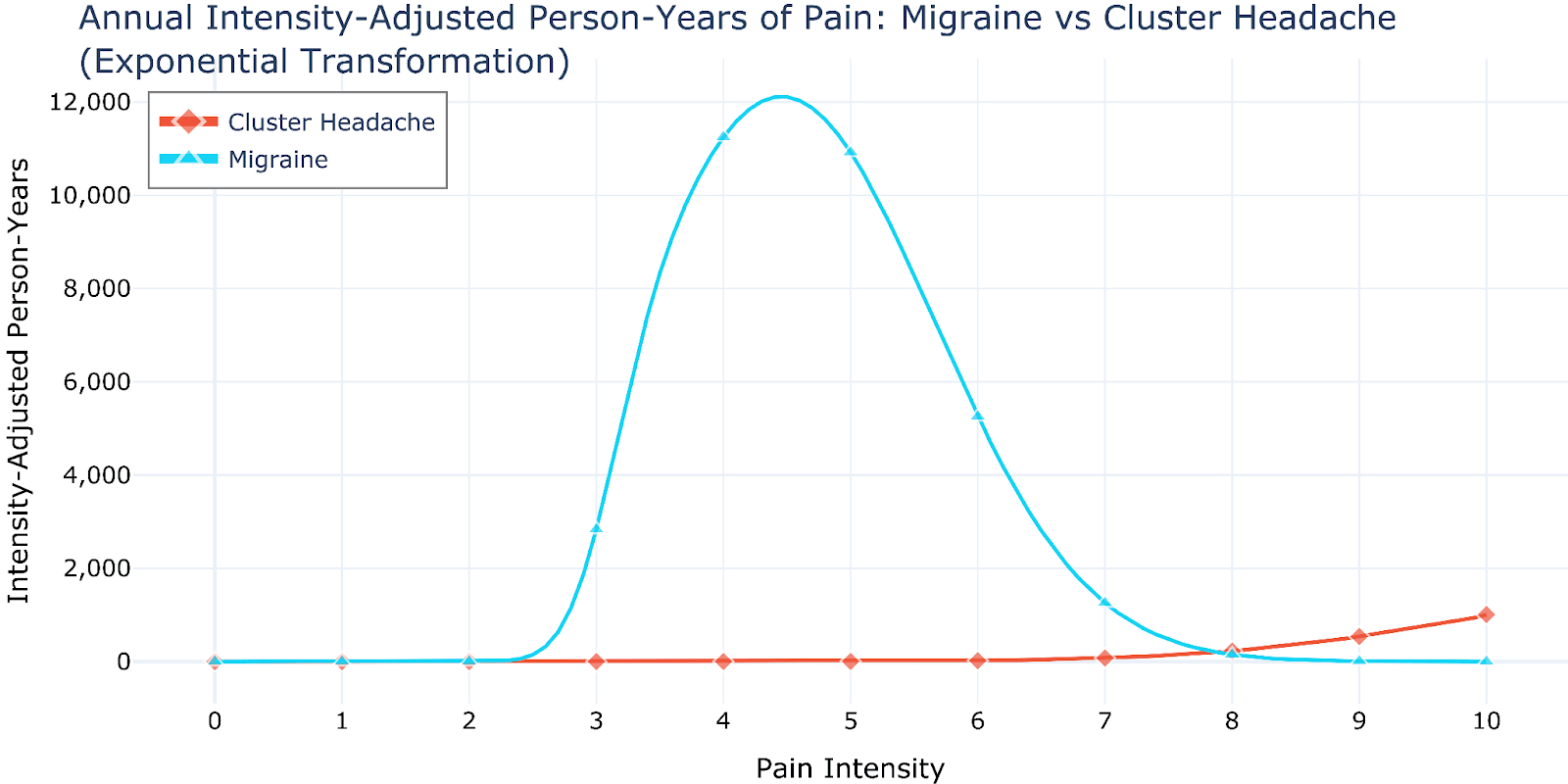
We can now ask: How much more heavily would we have to weigh intense pain compared to mild pain such that the intensity-adjusted burden of cluster headaches is larger than that of migraines? Or, referring to Figure 1, how steep does the weighting curve have to be, where 10/10 pain gets a weight of 1.0? Figure 4a shows the annual intensity-adjusted person-years assuming an exponential transformation proportional to eˣ. Note how the curves get compressed down for lower pain intensity values, causing the high-intensity pain values to become more prominent. However, even this exponential transformation is not steep enough to cause the overall burden (area under the curve) of cluster headaches to be larger than that of migraine. For this choice of migraine parameters, the intensity transformation would have to scale as ~6ˣ for the burden of cluster headaches to dominate (Figure 4b). This would mean, for example, that:
- Pain at 7/10 would get a weight of 0.005
- 8/10 pain a weight of 0.03
- 9/10 pain a weight of 0.1821
Our simulations also allow the user to ignore pain below 7/10 and focus on the intensity reweighting for the higher end of the pain scale. In this regime, much less steep transformations lead to cluster headaches dominating the total global burden. That is, one need not make strong assumptions about the relative importance of 7/10 pain compared to 10/10 pain (but at the cost of giving no weight to pain below 7/10). Using the same parameters as above, a transformation that gives:
- 7/10 pain a weight of 0.17
- 8/10 pain a weight of 0.32
- 9/10 pain a weight of 0.58
would result in a larger burden for cluster headaches (i.e., the weight scales roughly as 2x).
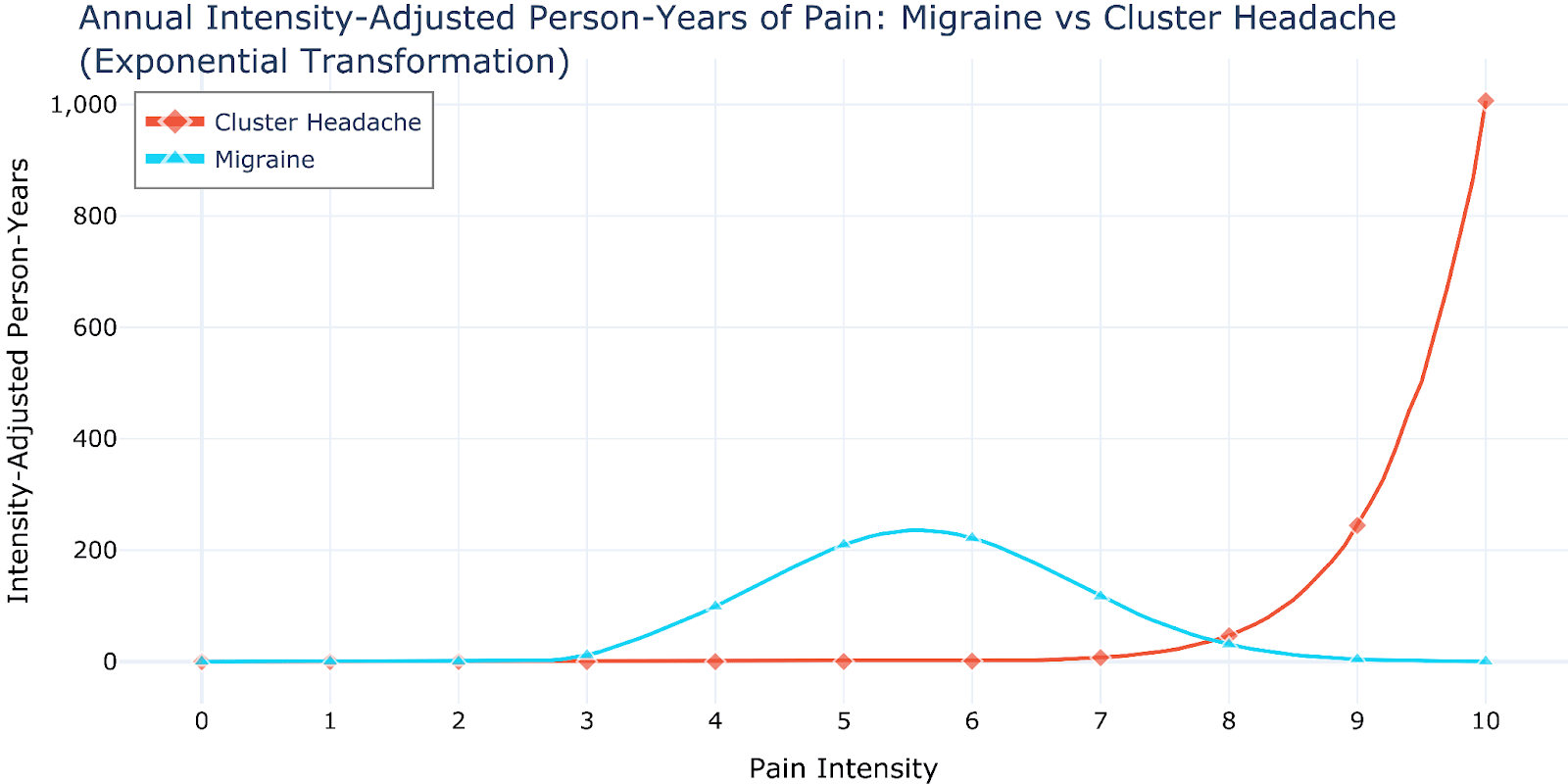
One might debate whether aggregating different pain intensities into a single metric—however heavily one decides to weigh extreme pain—is necessary or philosophically sound. Indeed, under minimalist axiologies or lexical views (Ajantaival 2024), one might decide to focus one’s efforts on reducing the most extreme forms of suffering (say, involving pain at a level of 9/10 or higher) regardless of whether there also exist other large amounts of milder suffering. Under this lens, relieving cluster headache suffering clearly takes priority over relieving migraine suffering. Whether cluster headaches are the top source of extreme suffering in humans worldwide is still unclear, but ongoing research will hopefully shed light on this question.22
3.3. Ceiling Effects
There are at least three major challenges when trying to quantify the pain intensity of various conditions:
- As mentioned in the previous section, patients with different pain conditions might interpret the scale differently (such as migraine patients who have never experienced the pain of cluster headaches). For example, imagine that a patient with both cluster headaches and migraines learns that migraine patients rate migraine pain at an average of 8/10. When asked to rate cluster headache pain, the cluster headache patient might instinctively think “12/10,” but they would answer “10/10” since that’s the highest score possible.23
- The distribution of answers to the question “How intense is pain from cluster headaches?” (or other conditions) will differ from the distribution of time actually spent at different pain intensities (i.e., how painful and how long each individual attack was, using headache diaries). Data on the former is more common and easier to gather (such as the survey by (Burish et al. 2021)).
- Individual patients themselves might have difficulties assessing the severity of each attack, for example due to recall bias or because what they thought was a 10/10 gets surpassed in future, even more severe attacks.
In each of these cases, there is a ceiling effect that distorts the true underlying distributions. A useful analogy would be asking university students to take an elementary school test, and getting an average score of 97/100. That average should not be interpreted as “slightly below 100” but rather as “much higher than what the test can measure, plus some room for minor mistakes.24”
A prediction of ceiling effects is that we should expect many values to cluster at the scale maximum, such as in the Burish et al. (2021) survey (and to some extent in the prospective reports from Table 1).
While a full treatment of this problem could be the subject of a separate research project, we can hint at potential approaches. For instance, one could assume an underlying normal distribution that extends beyond 10/10. Then, using statistical techniques (such as the tobit model), one could try to reconstruct the underlying distribution using (part of) the measured data. Figure 5 illustrates this approach.
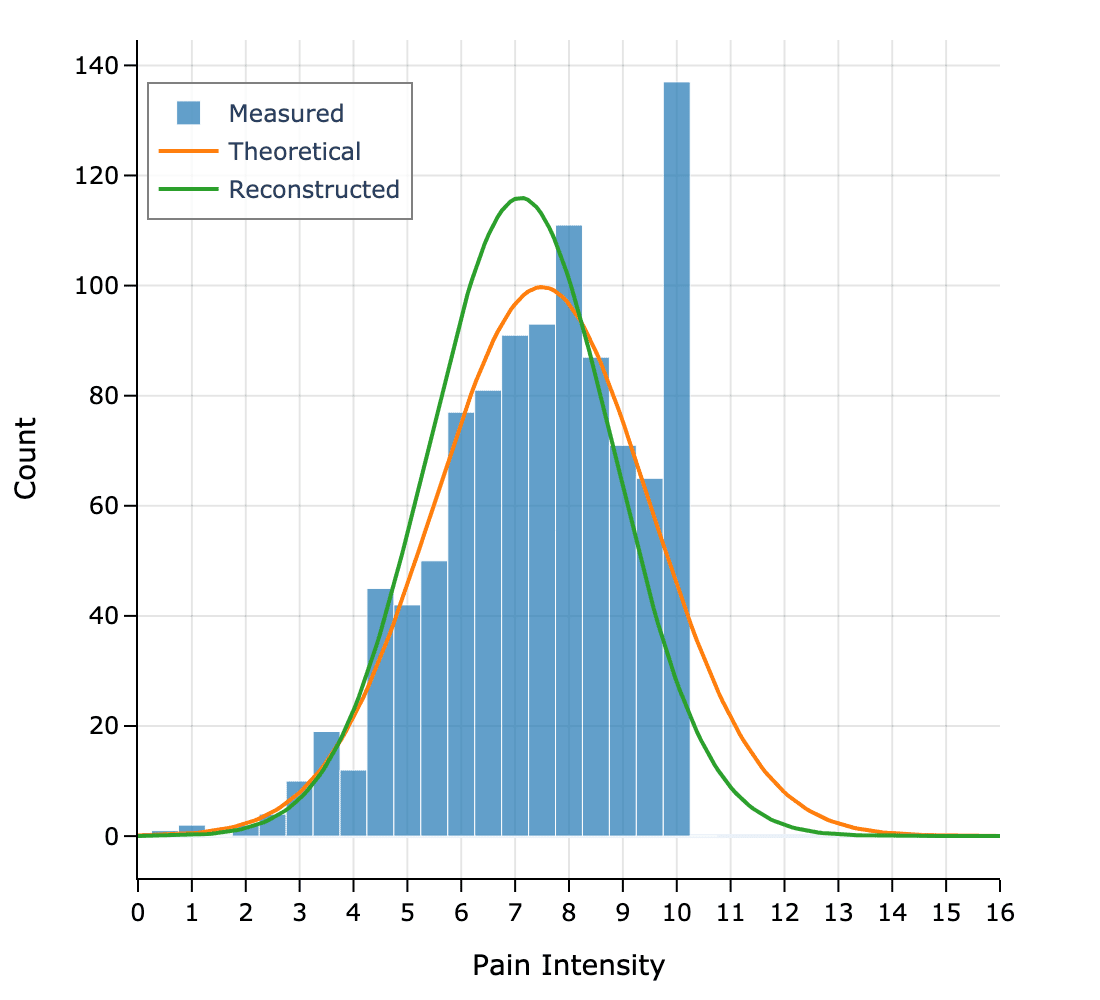
Incorporating ceiling effects would allow for more fair comparisons across conditions and a more accurate calculation of pain burden for extremely painful conditions. Indeed, we expect that our intensity calculations from Section 2.4 (based on a truncated normal distribution) lead to underestimating the total burden calculations—and it is precisely the behavior at the far end of the scale that we argue has the most weight. The resulting Figure 4 would look smooth as opposed to having an unnatural peak at the end, allowing us to capture the behavior of the underlying long tail fully. The overall case for prioritizing cluster headaches would be strengthened.
How exactly to capture such effects in patient data is a question for further research. One could consider giving patients the opportunity to enter scores higher than 10 in their diaries if their assessment of the pain evolves over time. Also, since patients who have had the condition for longer are better calibrated about the nature of the pain, their assessments could be weighted more heavily. Collecting data on the differences in relative, subjective intensity of attacks would also be valuable.
4. Recommendations and Conclusions
Our simulations suggest that cluster headaches cause a substantial amount of extreme human suffering globally—nearly 5 million Days Lived with Extreme Suffering (≥9/10 pain) per year. The fact that the prevalence of cluster headaches is much lower than that of other major diseases is actually advantageous and presents an attractive opportunity: we can get rid of a significant proportion of the most extreme human suffering worldwide at a small fraction of the cost of addressing more prevalent conditions. We invite readers to think ambitiously and recognize that reducing global cluster headache suffering by more than, say, 80% is achievable within a few years using currently available interventions.
Another reason to be optimistic about our ability to significantly reduce the burden of extreme suffering from cluster headaches is the low cost of some of the emerging treatments. As an example, an attack (roughly an hour long) could be aborted with anywhere between 3–20mg of N,N-DMT, costing as little as $1–6 per dose (assuming 0.5g cost $150). This excludes costs of research, policy reform, and implementation, but it gives us a sense of what’s possible (see also (Frerichs 2019) for further discussions).
Based on our findings, we offer several recommendations for different stakeholders:
For Philanthropists and Donors:
- Consider funding research into better treatments, particularly those involving indoleamines given their promising efficacy data (cf. Section 1.2, “Treatment and Prevention”). RCTs could be done in countries where these substances are legal.
- Support advocacy organizations working to improve access to existing treatments, especially in developing countries where access is severely limited. In particular, consider supporting Clusterbusters25, which provides resources and support to cluster headache sufferers. Clusterbusters plays a crucial role in raising awareness, facilitating patient connections, and advocating for research, with a very limited budget.
- Fund research to better quantify the burden of extreme suffering from various conditions to help prioritize interventions (such as work done by OPIS or QRI).
- Support organizations working on drug policy reform to enable research and treatment with currently restricted substances.
- Consider supporting retreat centers where promising psychedelic therapies can be offered to cluster headache patients legally and with substantial psychological and educational support (e.g., Eleusinia26).
For Researchers:
- Conduct more systematic studies comparing the intensity of different painful conditions using consistent methodologies.
- Develop and validate better metrics for measuring extreme suffering that account for the heavy-tailed nature of pain intensity.
- Conduct cost-effectiveness analyses of various interventions, including “busting” with psychedelics and other promising treatments, to inform funding decisions and maximize the impact of philanthropic efforts.
- Research the epidemiology of cluster headaches in developing countries, where data is currently limited.
- Research the underlying pathophysiology of cluster headaches, particularly their seasonal and circadian patterns, to develop more targeted treatments.
- Improve diagnostic tools and criteria to enable earlier diagnosis and treatment, since misdiagnosis and delayed diagnosis are common and lead to prolonged suffering.
For EA Organizations:
- Include cluster headaches in cause prioritization frameworks, particularly those focused on reducing extreme suffering.
- Consider launching dedicated funding initiatives and incubating new charities for cluster headache interventions.
- Develop networks connecting researchers, clinicians, and patient advocacy groups.
For Policy Advocates:
- Push for regulatory changes to allow ready medical access to restricted indoleamines, including through compassionate use provisions.
- Advocate to include cluster headaches in national and international health priorities.
- Work to improve insurance coverage for existing treatments, such as oxygen therapy and triptans.
For everyone else:
- Help raise awareness about the severity of cluster headaches.
- Consider directing charitable donations to organizations working on cluster headache relief in particular or meta work on extreme suffering more generally.
- Support advocacy efforts for better research funding and treatment access.
Acknowledgements
I’m particularly grateful to Andrés Gómez Emilsson for suggesting I work on this project, for feedback and discussions, and for bringing my attention to this problem through his previous research. I’m also grateful to Jonathan Leighton, Teo Ajantaival, Stefan Torges, Mark J. Burish, Hunter Meyer, Jim Buhler, Lucius Caviola, Clare Diane Harris, and Imma Six for their constructive feedback and encouragement. I thank Polaris Ventures for financially supporting this project.
Pain Research, Global Health, Cluster Headaches, Psychedelics, Heavy-Tailed Valence, N,N-DMT, Burden of Disease, Effective Altruism
Rossi et al. (2018) published a series of extracts from stories of European cluster headache patients who recount what it’s like to live with the condition (highly recommended). The website clusterheadaches.com also features testimonials by patients. This YouTube playlist is a compilation of videos of patients during attacks (disturbing). This artistic rendition (drawing) may be illustrative. Finally, the active, public Facebook group Cluster Headache Patients as well as r/clusterheads are a good place to get a sense of the daily struggles of cluster headache sufferers.↩︎
While we focus on simple aggregation across individuals and time, this work can be generalized to explore more elaborate assumptions, such as how suffering might cluster temporally or aggregate differently in single individuals, as well as the role of mixed valence (Gómez-Emilsson, 2023).↩︎
The remission period cut-off has been revised to 1 month (ICHD-3, 2013) but most papers we analyzed use the 3-month cut-off.↩︎
At the same time, the predictability can also help patients prepare better, especially if they have access to treatment options.↩︎
However, the survey did not ask whether intravenous or spinal/epidural anesthesia was used.↩︎
An attempt to estimate the DALY disability weight for cluster headaches can be found in Sharma et al. (2020), who suggest 0.624. Stovner et al. (2007) have suggested using reported pain as a proxy for the disability weight of headache disorders, but this alone wouldn’t be enough to address the concern raised by the HTV hypothesis.↩︎
Sharma et al. (2020) have made a similar observation: “There is also a seemingly strange result: the disability weights for terminal cancer patients with vs without pain relief are implausibly similar – 0.569 vs 0.540 – implying that cancer without pain relief is barely worse. This is especially odd considering that multiple randomized controlled trials have captured the significant effect opioids have on pain (see Wiffen et al., 2017 and Appendix 1).“↩︎
The authors don’t specify what age group qualifies as “adult”. For our simulations, we’re assuming ages 18+, for which the world population is 5,728,759,000 according to the UN. While the mean age of onset is somewhere between 23 and 34 years, the range spans 6 to 75 years (Kim et al., 2023). This would mean that 3.03 million adults worldwide will suffer from cluster headaches in a given year (CI: 1.49 million, 5.44 million). We also note that the authors didn’t specify whether they controlled for the age pyramid in each country, which could also affect the prevalence calculations.↩︎
The very large values reported for the standard deviation of remission periods relative to the mean (e.g. in Rozen et al., 2001) is indicative of a right-skewed distribution, possibly indicating many patients having shorter remissions and a few having very long ones.↩︎
See anecdotal evidence of patients going for a year or longer without any remission here.↩︎
See also further evidence of the long-tail distribution of annual attack frequency in Gómez-Emilsson (2019a), which could be partly or largely explained by the fraction of chronic patients with very short remission periods.↩︎
Although Gaul et al. (2012) report no significant difference in the retrospective reports of their cohort.↩︎
Although Snoer et al. (2018) found that untreated attacks were shorter in the prospective reports of their cohort. This is likely due to the fact that patients might decide not to use abortive treatment if they notice that the attack is mild (an observation also made by Hagedorn et al., 2019), and milder attacks tend to be shorter. 95% of the participants in Snoer et al.’s study had access to and used abortive treatment.↩︎
Plus Hagedorn et al. (2019), but they followed just one patient (for six years).↩︎
“The pain usually stays at maximal intensity for the duration of the attack, although it may wax and wane slightly, or be punctuated by super-intense stabs of pain.” (Nesbitt & Goadsby, 2012)↩︎
“Within a few minutes these symptoms became accentuated, assuming the character of real pain. This was usually very intense within 10-15 min. When the patient experienced maximum pain it was felt to be excruciating and generally occurred without fluctuations. Sometimes there were short repeated exacerbations of pain added to the continuous basic headache.” (Ekbom, 1975)↩︎
This metric might be somewhat analogous to the Suffering-Adjusted Life Years (SALY) metric suggested by Knaul et al. (2018) to quantify the burden of serious health-related suffering (SHS), but there are notable differences (e.g., the authors suggest including estimates of the value to the patient and their family of averting suffering), so we prefer not to use this term.↩︎
There is little data on the availability of treatments for cluster headache patients worldwide, so we made the following assumptions. Rossi et al. (2020) estimated that 47% of patients in the EU had full access to treatments, while 35% had limited access and 18% lacked access. Assuming that (a) these numbers are representative of developed countries worldwide, (b) ~15% of the world population lives in developed regions, ~25% of the world population lives in intermediate regions, and 60% of the world population lives in developing regions, (c) patients in intermediate regions have ~25% complete access, ~40% restricted access, and ~35% lacking access, while (d) patients in developing regions have ~10% complete access, ~30% restricted access, and ~60% lacking access, and (e) ~50% of patients with “restricted” access have access to treatment while ~15% of patients with “lacking” access have some access to treatment, we arrive at a global estimate of 43%. This parameter can be adjusted in our simulations.↩︎
As a reference, ischemic heart disease contributed 188 million DALYs and malaria contributed 55 million.↩︎
For the reasons discussed earlier, these numbers don’t necessarily reflect the average pain of attacks—they are an all-things-considered evaluation of the pain, which overestimates the actual pain distribution for both migraine and cluster headache.↩︎
The resulting scaling as 6x would mean that the 0–10 scale would have to span 4 orders of magnitude. While Gómez-Emilsson & Percy (2023) suggest the scale spans “at least two orders of magnitude”, private communication with the authors indicates their central estimates might be closer to 4 orders of magnitude, with uncertainty ranging from 2 to 8 OOMs.↩︎
An ongoing study by the Organisation for the Prevention of Intense Suffering (OPIS) aims to quantify the global burden of extreme suffering from all sources. Lack of access to pain relief for terminal or life-threatening illnesses (especially in developing regions) is a strong candidate, potentially causing more extreme human suffering than any other single source: More than 25 million people who died in 2015, including 2.5 million children, experienced “serious health-related suffering”, much of which is easily treatable (Knaul et al., 2018).↩︎
In fact, testimonials such as the following are easy to come by: “Imagine how it feels to be subjected to a knife attack on your head, like someone boring a screwdriver into your eye over and over again, sometimes for hours. […] On a scale of one (no pain) to ten (worst imaginable pain), you rate your pain at eleven and more.” (Rossi et al., 2018)↩︎
I thank Andrés Gómez Emilsson for pointing out the ceiling effect and suggesting this analogy.↩︎
While there are no detailed analyses on the effectiveness of their work, the existing data on the effectiveness of indoleamines, together with the fact that Clusterbusters are the main advocates of this intervention (and of cluster headache relief more generally), makes them stand out as one of the most promising organizations to support. More in the 2020 OPIS policy paper.↩︎
These two interviews with the founder of Eleusinia could be informative: Interview 1, interview 2.↩︎